struggling with vulvodynia?
What is Vulvodynia?
The medical definition for vulvodynia is vulvar pain that has been present for at least three months, that does not have any clear cause, and can have potential associated factors. What exactly does this mean?
Essentially the medical definition is saying that your vulva hurts, it’s been lasting for more than three months, everything looks normal with your tissue, and no one knows why you’re having pain.
Within vulvodynia, there are different descriptors that we can use to further describe things:
Localized (meaning a specific area, such as clitorodynia (pain in the clitoris) or vestibulodynia (pain in the vestibule)
Generalized (no particular area)
Mixed (meaning both localized and generalized)
Provoked (the pain only occurs with certain activities such as contact of the area or pelvic insertion/pelvic penetration)
Spontaneous (the pain has no clear cause)
Mixed (the pain has no clear cause but can also occur with specific instances or activities)
Onset:
Primary (pain has been present since the first sexual attempt)
Secondary (you were previously able to have sex pain-free before the pain started)
How Common is Vulvodynia?
Vulvodynia is considered to be a chronic condition that affects anywhere between 8-16% of people that identify as female at some point in their lifetime.
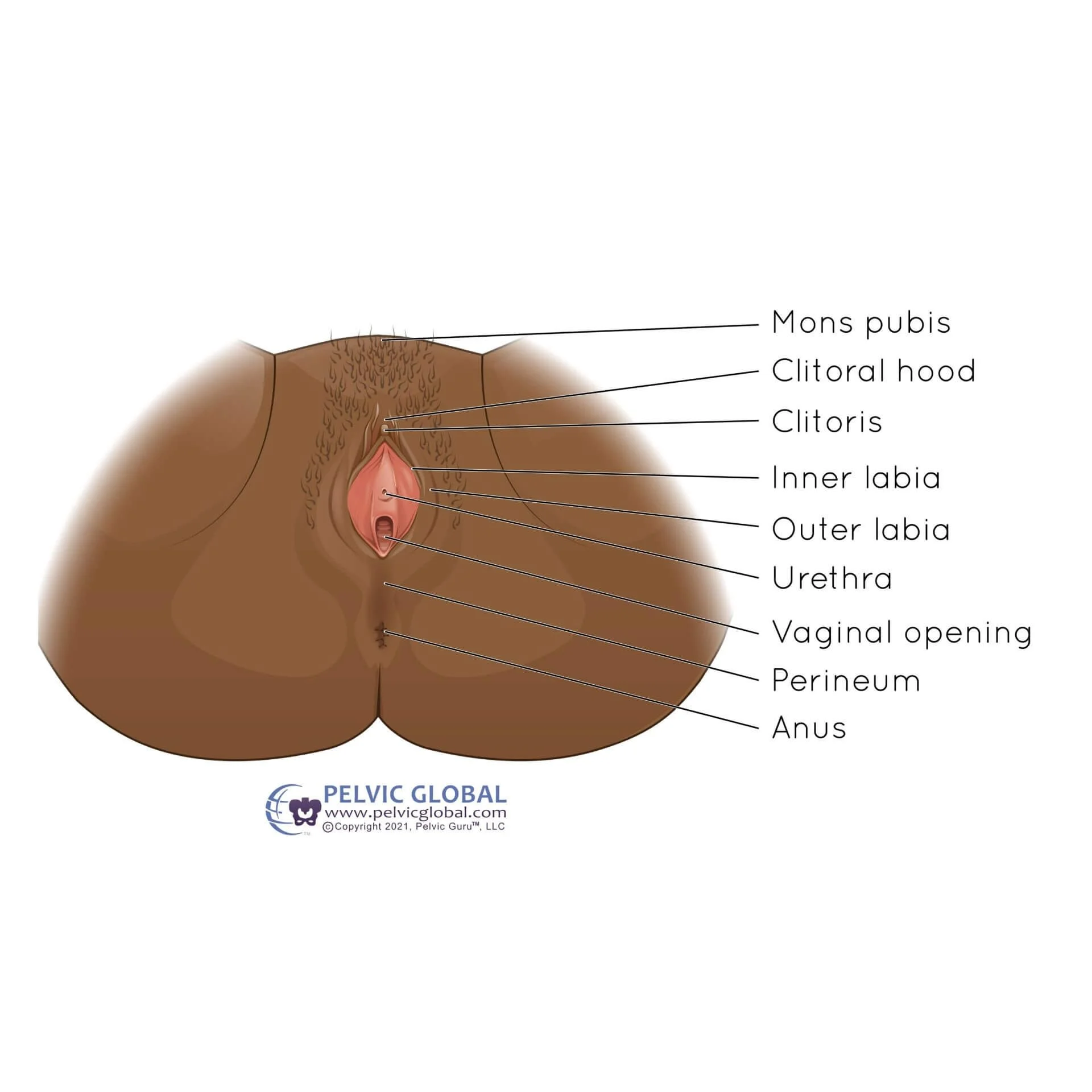
This image shows the vulva which is composed of the mons pubis, outer and inner labia (labia majora and minora), clitoris, and the hymen.
Common Symptoms of Vulvodynia
So what does it feel like if you are struggling with vulvodynia? You may experience:
Burning or pain at the vaginal opening during pelvic penetration
Vulvar burning, stabbing, or shooting pain'
Urgency with urination
Frequent urination
Pain with urination
Difficulty starting the flow of urine when going to the bathroom to pee
Pain in the abdomen and pelvic region
Back pain
Burning, swelling, and hypersensitivity of the vulva
Changes with orgasm
Foot and leg pain
Pelvic Floor Physical Therapy Recommendations for Vulvodynia
Okay, so now that we know what vulvodynia is and how it can impact a person, most clients ask me what is available for treatment. Here’s what we know:
Personal hygiene practices matter. A lot of times clients that I work with who are struggling with vulvodynia are using different products at the vulvar tissue that may actually be making their symptoms worse.
I usually provide a ton of education of wearing cotton underwear which are more breathable than synthetically based products and tend to be less irritating to the genital tissue. It’s also recommended to not wash the vulvar or vaginal tissue with soap or do any other form of “hygienic” practices like douching or using fragrances. Your vulva and vagina only need to be cleaned with lukewarm water…no soaps or fragrances. The vulvar tissue is sensitive and using different products marketed by mainstream media can potentially be a trigger for your vulvodynia symptoms. A vulva and vagina is supposed to smell exactly like that: a vulva and vagina.
This is a hill I will die on. Hormones are important. Oftentimes clients that I work with who are struggling with vulvodynia are in different seasons of life (think perimenopause, menopause, after menopause, pregnancy, chest feeding, taking hormonal birth control, gender affirming hormonal treatment, cancer treatment) where changes in hormones can be a trigger for symptoms relating to vulvodynia. Then upon visual assessment of the tissues of the vulva and vestibule we find significant irritation of these tissues which can potentially be a cause of vulvodynia. Sometimes for these clients that I am working with by simply getting a prescription from their gynecologist for a topical estrogen or DHEA cream to apply to the tissues can be a total game changer. With regular use of these hormonal supplements once we resolve the irritation of the tissues the symptoms relating to vulvodynia may magically go away too. YAY!
Stress and nervous system upregulation plays a role. We know that the majority of folks with pelvic pain also have an issue with a dysregulated nervous system.
Mmmkay. What does this mean? The definition of pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage. Pain is our body’s way of communicating with us and trying to protect us when it perceives something as threatening or that can potentially harm us. So your pain is very real. But often times with pain and for clients with persistent pelvic pain we can start to believe that there is damage to our body or tissues if pain is present, even if there is not.
Hear me out. If we think about pain as our body’s way of communicating with us it can be helpful with improving pain by getting curious with why our body is telling us that something is threatening. The research literally shows us that this curiosity can help us to improve the pain that we are experiencing.
Pain science education frequently gets a bad reputation that oftentimes folks walk away feeling like they are being told that their pain isn’t real. Which is not true. But it’s helpful to know that your pain is both real and that your pain system is hypersensitive contributing to your pelvic pain. We also know with pain science that how you see, feel, and think about your pain can actually make your pelvic pain worse. Keeping this in mind, there are many ways that you can manage your pain by thinking about things more broadly instead of focusing on the vulvar tissues alone. It is also important to know that your pain is changeable and that there is hope that things can improve and that pain improvement is a very real and achievable goal when it comes to vulvodynia.
Keeping all of these things in mind is incredibly empowering for clients who I work with who are struggling with vulvodynia and in and of itself can make huge changes in their vulvar pain.
Tight muscles can be contributing to your vulvodynia symptoms. Sometimes from having pain in the pelvic and vulvar tissues, regardless of whether it is in part from a dysregulated or hypersensitive pain system, issues with hormones, using products in the vulvar region that could be causing increased vulvar sensitivity, or a combination of these things, can cause increased tension in the pelvic floor muscles which can further contribute to pain associated with vulvodynia.
Pelvic floor muscle tension or tightness is something that I see a lot with clients who are struggling with persistent pelvic pain associated with vulvodynia. Fortunately, there are so many things that we can do to help with this through pelvic floor physical therapy treatment including:
Manual therapy techniques at the pelvic floor muscles such as dilator therapy, using a pelvic wand, or with your pelvic floor physical therapist using hands-on techniques during appointments to help gently stretch and lengthen the muscles in the pelvic region which helps to desensitize the muscles so that touch is perceived as touch alone and is not painful
Downregulation techniques for your nervous system: as a pelvic floor physical therapist I use a lot of techniques focusing in the areas of the head, neck, and jaw where the vagus nerve originates from which plays a big role in the functioning of the pelvic floor muscles. Sometimes for clients that have a lot of discomfort in the pelvic region where the nervous system is super ramped up we can start first by working in more neutral areas like the head and neck which can still make a big impact and improvement in pelvic pain.
Taking a whole body (and whole person) approach: not only do we address the pelvic region when it comes to pelvic pain during pelvic floor physical therapy appointments, but I am a huge advocate of treating the whole person sitting in front of me. I like to think outside of the box with all aspects of your life that could potentially be contributing to your pelvic pain (Think: What is your workplace setup like? What are your stress levels like? What is your diet and physical activity levels like?) as well as things outside of your pelvis and pelvic floor in the surrounding areas of the body that could also be contributing to your pain. Not only do we talk about these things and assess the surrounding areas of the body like the hips, low back, and sacroiliac joint but we address any issues that may arise that are potentially feeding into the pain response associated with vulvodynia.
Have questions or feeling on the fence about whether or not pelvic floor physical therapy is for you? If you’re looking for treatment for vulvodynia or are struggling with pelvic floor issues and you’re located in Durham, North Carolina I would love to work with you! Reach out to me here to tell me a little more about what is going on so we can chat more and get the process started. Live outside of the state of North Carolina? I also offer virtual appointment options to provide more accessible care to those seeking out pelvic floor treatment for vulvodynia.
Struggling with vulvodynia or other pelvic floor conditions? Check out my website here to see what other conditions I treat as a pelvic floor physical therapist.
Dr. Brook Orvis (she/her) is a Board-Certified Women’s Health and Pelvic Floor Physical Therapist, Duke Residency-Trained in Women’s Health, and the owner of Flora Physical Therapy. As a momma to a spirited toddler, she understands the difficulty of being a parent while prioritizing self-care, including caring for your body and pelvic floor. She believes that pelvic floor therapy is for everyone and is passionate about providing accessible treatment options for birthing people, men, women, kids, and the LGBTQIA+ community so that they can take better care of themselves and receive equitable care. She loves educating and empowering clients to take charge of their body and health and to not accept leaking of urine, prolapse, pelvic pain, pain during sex, and core weakness as a normal part of being a human.